ORTHOPAEDIC INFO
Our institute specializes in Joint Replacement, Hip, Knee, Shoulder, Elbow, Small joints of hand, Arthroscopic Surgery (ACL, PCL, MCL) & more
- Orthopaedic Ailments
- Arthritis
- Arthroscopy
- Trauma
- Joint Replacement
Orthopaedic Ailments
Osteoporosis is a disease of bones that leads to an increased risk of fracture. Osteoporosis literally means ‘porous bones’. In osteoporosis the bone mineral density (BMD) is reduced, bone microarchitecture is disrupted, and the amount and variety of proteins in bone is altered. Osteoporosis is defined by the World Health Organization (WHO) in women as a bone mineral density 2.5 standard deviations below peak bone mass (20-year-old healthy female average) as measured by DXA; the term “established osteoporosis” includes the presence of a fragility fracture.. Osteoporosis is most common in women after menopause, when it is called postmenopausal osteoporosis, but may also develop in men, and may occur in anyone in the presence of particular hormonal disorders and other chronic diseases or as a result of medications, specifically glucocorticoids, when the disease is called steroid- or glucocorticoid-induced osteoporosis (SIOP or GIOP). Given its influence in the risk of fragility fracture, osteoporosis may significantly affect life expectancy and quality of life. Disease of the parathyroid glands (hyperparathyroidism) is also a major cause of osteoporosis. Hyperparathyroidism should be high on the list of causes in any patient with severe osteoporosis, osteoporosis occurring at a young age, or osteoporosis in a male. Over consumption of dietary protein is another often neglected cause of osteoporosis. The excess protein causes calcium to be taken from the bones and excreted in the urine. . Osteoporosis can be prevented with lifestyle changes and sometimes medication; in people with osteoporosis, treatment may involve both. Lifestyle change includes exercise and preventing falls as well as reducing protein intake. Medication includes calcium, vitamin D, bisphosphonates and several others. Fall-prevention advice includes exercise to tone deambulatory muscles, proprioception-improvement exercises; equilibrium therapies may be included. Exercise with its anabolic effect, may at the same time stop or reverse osteoporosis. Osteoporosis is a component of the frailty syndrome.
Arthritis
Arthritis is a joint disorder featuring inflammation. A joint is an area of the body where two different bones meet. A joint functions to move the body parts connected by its bones. Arthritis literally means inflammation of one or more joints. Arthritis is frequently accompanied byjoint pain. Joint pain is referred to asarthralgia. There are many types of arthritis (over 100 identified, and the number is growing). The types range from those related to wear and tear of cartilage (such as osteoarthritis) to those associated with inflammation resulting from an overactive immune system (such as rheumatoid arthritis). Together, the many types of arthritis make up the most common chronic illness in the United States. The causes of arthritis depend on the form of arthritis. Causes include injury (leading to osteoarthritis), metabolic abnormalities (such as gout andpseudogout), hereditary factors, the direct and indirect effect of infections (bacterial and viral), and a misdirected immune system with autoimmunity (such as in rheumatoid arthritis andsystemic lupus erythematosus). Arthritis is classified as one of the rheumatic diseases. These are conditions that are different individual illnesses, with differing features, treatments, complications, and prognoses. They are similar in that they have a tendency to affect the joints, muscles, ligaments, cartilage, and tendons, and many have the potential to affect other internal body areas. Symptoms: Symptoms of arthritis include pain and limited function of joints. Inflammation of the joints from arthritis is characterized by joint stiffness, swelling, redness, and warmth. Tenderness of the inflamed joint can be present Many of the forms of arthritis, because they are rheumatic diseases, can cause symptoms affecting various organs of the body that do not directly involve the joints. Therefore, symptoms in some patients with certain forms of arthritis can also includefever, gland swelling (swollen lymph nodes), weight loss, fatigue, feeling unwell, and even symptoms from abnormalities of organs such as the lungs, heart, or kidneys.
Arthroscopy
Arthroscopy is a surgical procedure by which the internal structure of a joint is examined for diagnosis and/or treatment using a tube-like viewing instrument called an arthroscope. Arthroscopy was popularized in the 1960s and is now commonplace throughout the world. Typically, it is performed by orthopedic surgeons in an outpatient setting. When performed in the outpatient setting, patients can usually return home after the procedure The technique of arthroscopy involves inserting the arthroscope, a small tube that contains optical fibers and lenses, through tiny incisions in the skin into the joint to be examined. The arthroscope is connected to a video camera and the interior of the joint is seen on a television monitor. The size of the arthroscope varies with the size of the joint being examined. For example, the knee is examined with an arthroscope that is approximately 5 millimeters in diameter. There are arthroscopes as small as 0.5 millimeters in diameter to examine small joints such as the wrist. If procedures are performed in addition to examining the joint with the arthroscope, this is called arthroscopic surgery. There are a number of procedures that are done in this fashion. If a procedure can be done arthroscopically instead of by traditional surgical techniques, it usually causes less tissue trauma, results in less pain, and may promote a quicker recovery.
Trauma
Trauma: Any injury, whether physically or emotionally inflicted. “Trauma” has both a medical and a psychiatric definition. Medically, “trauma” refers to a serious or critical bodily injury, wound, or shock. This definition is often associated with trauma medicine practiced in emergency rooms and represents a popular view of the term. In psychiatry, “trauma” has assumed a different meaning and refers to an experience that is emotionally painful, distressful, or shocking, which often results in lasting mental and physical effects. Sports Medicine: Sports medicine is an area of health and special services that apply medical and scientific knowledge to prevent, recognize, manage, and rehabilitate injuries related to sport, exercise, or recreational activity
Joint Replacement
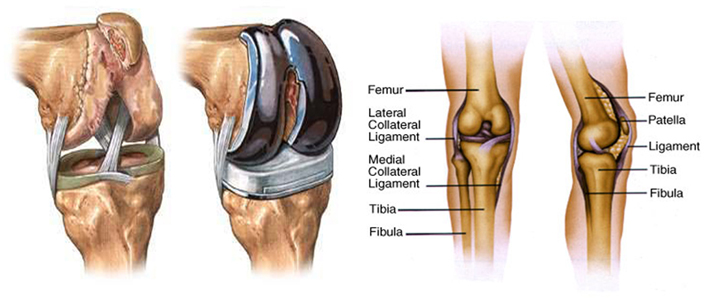
Joint replacement is the surgical replacement of a joint with an artificial prosthesis. A prosthesis is a device designed to replace a missing part of the body or to make a part of the body work better Joint replacements are performed under general or regional anesthesia in a hospital by an orthopedic surgeon. Some medical centers specialize in joint replacement, and these centers generally have a higher success rate than less specialized facilities. The specific techniques of joint replacement vary depending on the joint involved. joint replacement surgery, is a procedure of orthopedic surgery, in which the arthritic or dysfunctional joint surface is replaced with an orthopedic prosthesis. When joint replacement surgery occurs, the artificial surfaces of the joint replacement are shaped in such a way as to allow joint movement similar to that of a healthy and natural joint. A person who has injured or damaged their joint may experience extremely severe pain at the site of the joint. In certain instances when the pain is extremely severe, one may “avoid using the joint, weakening the muscles around the joint and making it even more difficult to move the joint”[1]. In such a severe case, one may consider a Joint Replacement as a possible solution. Examinations and tests will be performed to assess the severity of the joint damage. If less invasive alternatives don’t alleviate pain and damage, Total Joint Replacement will be considered. When to Seek Medical Care Call your family doctor or orthopedist if you develop gradual pain that feels like slippage in your knee. This generally is an urgent problem, but not an emergency. Call your doctor if you notice unexpected drainage from or poor healing of a recent surgery, increasing swelling, or warmth. Go to the hospital’s emergency department if you experience any of the following: A fracture or dislocation after a fall New swelling Redness, or warmth at a joint suggesting infection Swelling, pain, or redness below your knee that suggests a clot in your vein (deep venous thrombosis or DVT) Procedures The doctor puts a tourniquet above the knee, than makes a cut to expose the knee joint. The ligaments surrounding the knee are loosened, then the shin bone and thigh bone are cut and the knee removed. The artificial knee is then cemented into place on the remaining stubs of those bones. The excess cement is removed, and the knee is closed. Hospital stays range from three to six days. In both types of surgery, preventing infection is very important. Antibiotics are given intravenously and continued in pill form after the surgery. Fluid and blood loss can be great, and sometimes blood transfusions are needed. Preparation Many patients choose to donate their own blood for transfusion during the surgery. This prevents any blood incompatibility problems or the transmission of blood-borne diseases. Prior to surgery, all the standard preoperative blood and urine tests are performed, and the patient meets with the anesthesiologist to discuss any special conditions that affect the administration of anesthesia. Patients receiving general anesthesia should not eat or drink for 10 hours prior to the operation. Aftercare Immediately after the operation the patient will be catheterized so that he or she will not have to get out of bed to urinate. The patient will be monitored for infection. Antibiotics are continued and pain medication is prescribed. Physical therapy begins (first passive exercises, then active ones) as soon as possible using a walker, cane, or crutches for additional support. Long term care of the artificial joint involves refraining from heavy activity and heavy lifting, and learning how to sit, walk, how to get out of beds, chairs, and cars so as not to dislocate the joint. Risks The immediate risks during and after surgery include the development of blood clots that may come loose and block the arteries, excessive loss of blood, and infection. Blood thinning medication is usually given to reduce the risk of clots forming. Some elderly people experience short term confusion and disorientation from the anesthesia. Although joint replacement surgery is highly successful, there is an increased risk of nerve injury. Dislocation or fracture of the hip joint is also a possibility. Infection caused by the operation can occur as long as a year later and can be difficult to treat. Some doctors add antibiotics directly to the cement used to fix the replacement joint in place. Loosening of the joint is the most common cause of failure in hip joints that are not infected. This may require another joint replacement surgery in about 12% of patients within a 15-year period following the first procedure. Normal results Over 90% of patients receiving hip replacements achieve complete relief from pain and significant improvement in joint function. The success rate is slightly lower in knee replacements, and drops still more for other joint replacement operations
Hip Joint Replacement
The surgeon makes an incision along the top of the thigh bone (femur) and pulls the thigh bone away from the socket of the hip bone (the acetabulum). An artificial socket made of metal coated with polyethylene (plastic) to reduce friction is inserted in the hip. The top of the thigh bone is cut, and a piece of artificial thigh made of metal is fitted into the lower thigh bone on one end and the new socket on the other.
The artificial hip can either be held in place by a synthetic cement or by natural bone in-growth. The cement is an acrylic polymer. It assures good locking of the prosthesis to the remaining bone. However, bubbles left in the cement after it cures may act as weak spots, causing the development of cracks. This promotes loosening of the prosthesis later in life. If additional surgery is needed, all the cement must be removed before surgery can be performed.
An artificial hip fixed by natural bone in-growth requires more precise surgical techniques to assure maximum contact between the remaining natural bone and the prosthesis. The prosthesis is made so that it contains small pores that encourage the natural bone to grow into it. Growth begins 6 to 12 weeks after surgery. The short term outcome with non-cemented hips is less satisfactory, with patients reporting more thigh pain, but the long term out-look is better, with fewer cases of hip loosening in noncemented hips. The trend is to use the non-cemented technique. Hospital stays last from four to eight days.
Both chronic osteoarthritis and rheumatoid arthritis commonly cause people to lose knee function to the degree that they need a knee joint replacement (total knee arthroplasty or TKA). But knee damage may also stem from injury or infection. Generally, people require a TKA a decade earlier due to rheumatoidarthritis as opposed to osteoarthritis

Knee Joint Replacement
Both chronic osteoarthritis and rheumatoid arthritis commonly cause people to lose knee function to the degree that they need a knee joint replacement (total knee arthroplasty or TKA). But knee damage may also stem from injury or infection. Generally, people require a TKA a decade earlier due to rheumatoidarthritis as opposed to osteoarthritis
- The most common problems with a knee joint replacement
- Fractures (breaks) of the new knee after a fall or other accident
- Pain from slippage and wear in the new joint
- Other less common problems
- Infection of the joint
- Dislocation, either complete or partial, of the new knee
- A blood clot in a vein (deep vein thrombosis) above or below the knee (Clots occur most commonly shortly after replacement surgery.)
Knee joint Replacement symptoms:
- Many people who fall after having a knee replacement break the bone below the new joint on which the new knee is anchored. Pain and swelling occur at or near the site of the knee joint replacement.
- Pain can occur gradually as the new joint develops wear patterns that interfere with the smooth function of your knee
- Slippage can cause bony surfaces to move opposite each other and cause pain.
- This pain increases the more steps you take and decreases when you sit
- This pain of movement differs from the normal start-up pain that occurs in the first 3-6 months after knee replacement and that decreases over the first few steps
- Infection will cause pain, along with frequent redness and swelling at the joint, even when you are at rest.
- Often fluid will collect at the knee joint from infection and cause a boggy swelling. Fluid may not accumulate with every infection
- Fever may occur.
- Dislocating the knee will cause pain
- Deformity of the joint will be obvious
- A dislocation may damage adjoining nerves, muscles, and blood vessels and impair their function. The popliteal artery, which carries the entire blood supply to your lower leg and foot, can be injured or pinched shut. Nerves to your lower leg can be cut or injured, causing your lower leg to become numb (paresthesia), weak (paresis), or paralyzed. Arteries can be partially or totally blocked, eventually causing pain, the lower leg to turn pale and cold, poor or no pulse, and the leg to swell
- Blood clots tend to form during the period (“post-op,” or “post-operatively”) when you cannot move following a knee replacement
- Clots become progressively less common with time.
- A clot in your vein generally causes new pain, swelling, or redness in your lower leg.
- The greatest concern is that the clot will travel through your veins and could lodge in your lung (pulmonary embolism).
